Virus sterilization by UVC radiation
Sterilization of viruses was investigated by a UVC radiation based prototype device developed by Captain Corrosion OÜ in the framework of Estonian Research Council project COVSG31 "Indoor cleaning from respiratory viruses by plasma technology".
The main inactivation mechanism for low-pressure UVC lamps is likely through viral genome damage (Lo et al. 2021). The Eilat virus (EILV) was used as a model to detect the virus inactivating effect of the UVC lamp. The use of EILV as an alphavirus in these experiments was justified by the fact that the virion structure of alphaviruses includes a membrane envelope of host cell origin that characterizes, inter alia, other groups of viruses pathogenic to humans, such as coronaviruses and influenza viruses. In addition, EILV is a safe pathogen for humans that can only infect insect cells, and therefore the performed tests are safe for the operator and allow the tests to be performed in a lower-risk laboratory (in this case the BSL2 laboratory).
EILV stock solutions with a concentration of 107 to 2.8 * 108 FFU/ml (focus forming unit) were applied to the experiments and applied to tissue culture dishes in a volume of 400 μl, which was then covered with a square piece of film with a side length of 40 mm. A low-pressure mercury vapor UVC lamp with 15 W power (Fig. 1) was used to irradiate the virus solutions applied to the dishes. The experiments were performed at distances of 0.8 m and 2.5 m, where the irradiations were performed for 5, 10 or 15 minutes. Three experiments were performed for all parameters.
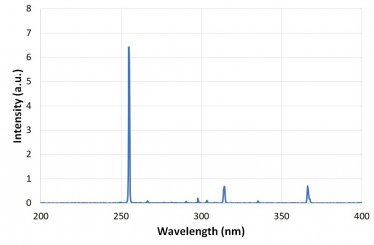
Figure 1. UV emission of Hg lamp with strongest emission line at 254 nm corresponding to UVC radiation.
Virus survival was determined by titration using a fluorescent focus formation method. The method was enabled by the mCherry coding sequence inserted into the recombinant EILV genome used in the experiments. The virus infected the mosquito Aedes albopictus cell line C6/36. A series of 10-fold dilutions were prepared for analysis of each sample and used to infect the cell culture. After infection, a cell culture medium was applied to the cell layers, which ensures that the virus only spreads to immediate neighboring cells in the cell dish. The infected cells were then incubated for an additional 72 h, during which time fluorescent cell foci were formed as a result of viral activity, which could be visualized under a fluorescence microscope and counted to determine titers. Calculated titers are in FFU/ml.
The test results are shown in Table 1, which summarizes the average titers of the three samples and where UV + represents the samples irradiated with UVC and the UV control levels. The percentage of viruses inactivated by the UVC lamp in a given time is also presented. At a distance of 0.8 m, 99.9% viruses were inactivated in 5 minutes and after 15 minutes all viruses are inactivated. At a distance of 2.5 m, the effect is much smaller, but about 93% of the viruses can be inactivated in 15 minutes.
Table 1. Proportion of inactivated viruses depending on the duration of UVC treatment.
|
Distance (2.5 m) |
Average titre of three samples (FFU/ml) |
Difference (%) |
|
UV+ 15 min |
3,60E+05 |
93,1 |
|
UV- 15 min |
5,20E+06 |
|
|
UV+ 10 min |
8,37E+05 |
84,3 |
|
UV- 10 min |
5,33E+06 |
|
|
UV+ 5 min |
3,91E+06 |
26,2 |
|
UV- 5 min |
5,30E+06 |
|
|
Distance (0.8 m) |
Average titre of three samples (FFU/ml) |
Difference (%) |
|
UV+ 15 min |
0,00E+00 |
100,1 |
|
UV- 15 min |
6,47E+06 |
|
|
UV+ 10 min |
7,33E+01 |
99,9999 |
|
UV- 10 min |
5,80E+07 |
|
|
UV+ 5 min |
6,60E+04 |
99,9 |
|
UV- 5 min |
5,70E+07 |
|
Figure 2 shows the inactivation of viruses on a logarithmic scale as a function of processing time. The virus inactivation by UVC radiation is often characterized by first-order inactivation kinetics model and therefore depends exponentially on the duration of UVC radiation. This is expressed as log10(N/N0) = -k t. The constant k characterizes the inactivation rate of the virus and its inverse value is the time constant (2.7-fold reduction time) for virus inactivation. The time constant for virus inactivation determined from the straight line is 1.67 min for 0.8 m and 13.3 min for 2.5 m. The difference is about 8 times. The UVC radiation intensity of a point source decreases inversely with the square of the distance, which is 0.64 m2 for 0.8 m and 6.25 m2 for 2.5 m. About ten times lower radiation dose at distance of 2.5 meters is in line with the 8-fold difference in time constant. Based on the time constant determined from the experiment, it can be estimated that UVC treatment of approximately 30 minutes is required to inactivate 99% of viruses at a distance of 2,5 m. Same inactivation is achieved in 3.3 minutes at the distance of 0.8 m.
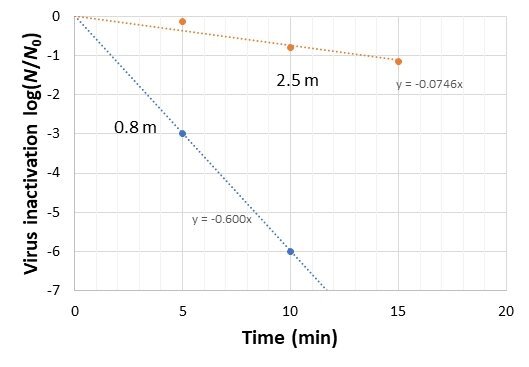
Figure 2. Virus inactivation as a function of time on a logarithmic scale. The coefficient indicates the characteristic rate of virus inactivation.
The estimated UVC dose required for 99% virus inactivation was approximately 10 mJ/cm2 when assuming the 30 % efficiency of the 15 W UVC lamp point source. This result is in line with other studies of virus inactivation (Ma et al 2021, Lo et al 2021, Tseng et al 2007) by UVC where 99% inactivation of various viruses including SARS-CoV-2 has been achieved in the UVC dose range of 2-10 mJ/cm2.
References:
C.-W. Lo, R. Matsuura, K. Iimura, S. Wada, A. Shinjo, Y. Benno, M. Nakagawa, M. Takei, Y. Aida, 2021 UVC disinfects SARS-CoV-2 by induction of viral genome damage without apparent effects on viral morphology and proteins, Sci. Reports 11 13804
B. Ma, P.M. Gundy, C.P Gerba, M.D. Sobsey, K.G. Linden, 2021, UV Inactivation of SARS-CoV-2 across the UVC Spectrum: KrCl* Excimer, Mercury-Vabor, and Light-Emitting-Diode (LED) Sources, Appl. Environ. Microbiol. 97 e01532-21
C.-C. Tseng, C.-S. Li, 2007, Inactivation of Viruses on Surfaces by Ultraviolet Germicidal Irradiation, J. Occ. Envrion. Hyg. 4, 400-405


